By Niklas Krausse, Magdalena Madej and Ouyang Yuan
Have you ever wondered where the new cells come from after an injury? How is it possible, that a scratch on our skin is replaced with new skin after a couple of days? It is said that time heals all wounds, but stem cells play a big role in many cases too.
Stem cells do much more than repair scratches though. Did you know that:
• 100 million new red blood cells are generated in our body every minute?1
• The lining of the small intestine is fully exchanged every 4 days?2
• The human epidermis (skin) is entirely replaced in 27 days on average?3
Maintenance (homeostasis) is one of the most important functions of stem cells, which help us keep our bodies in good shape and jump in when necessary, for example following injuries or infections. So, let’s take a closer look at these fascinating cells. In order to be classified as a stem cell, two fundamental criteria have to be met:
1. The cell is able to make new cells of their own kind (self-renewal)
2. The cell can change into a different cell type (differentiation)
Usually, stem cells live in a certain location in our body, called the niche or microenvironment. The niche consists of other cell types that protect and maintain the stem cells. Often, the niche cells communicate with the stem cells and provide instructions about what mature cell types are currently needed. However, if there is no urgent need for new supply, most stem cells tend to be in a non-active or dormant state. Stem cell dormancy helps to protect and prolong the life of these precious cells. Any kind of error in stem cells can have devastating consequences, since they can pass that error on to descending cells. These mistakes can be passed on to either new stem cells made by self-renewal, or differentiated cells originating from the “faulty” stem cell.
Stem cell types
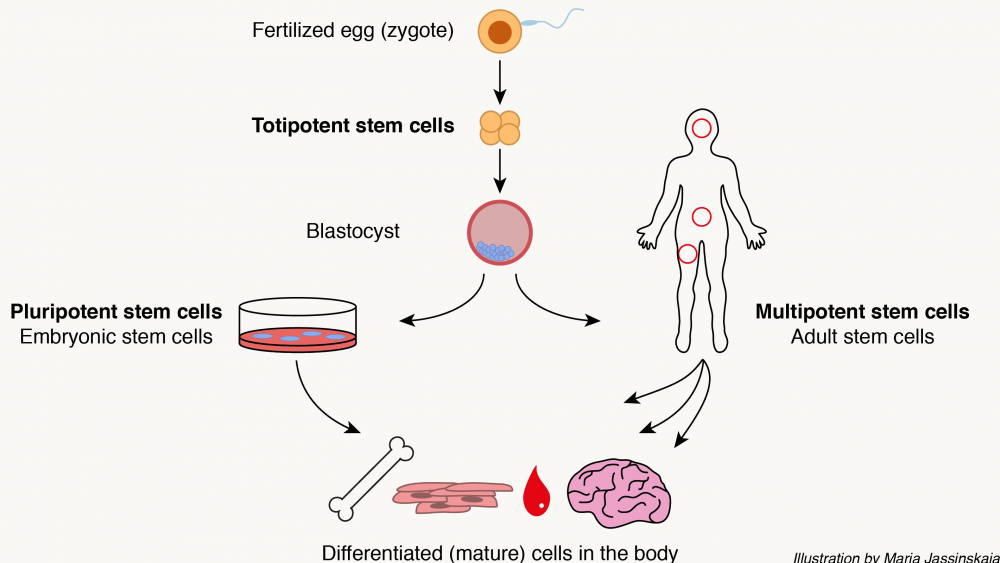
 Stem cells come in different flavors. Broadly, they can be categorized into three different types: Embryonic stem cells, adult stem cells, and induced pluripotent stem cells. They differ in their origin as well as how restricted they are in their potential to give rise to other cell types. In other words, their potency.
Stem cells come in different flavors. Broadly, they can be categorized into three different types: Embryonic stem cells, adult stem cells, and induced pluripotent stem cells. They differ in their origin as well as how restricted they are in their potential to give rise to other cell types. In other words, their potency.
Embryonic stem cells (ESCs)
Just like a human life, the stem cell story has its beginning with the union of a human sperm and egg. This leads to the formation of the most potent cell in human body, a zygote. The zygote is totipotent, which means that it is capable of creating any cell type in an organism, as well as extraembryonic tissues such as the placenta. The totipotent state lasts for 4 days until the zygote has developed into a blastocyst, which could be described as a tiny ball with embryonic stem cells inside. The embryonic stem cells are pluripotent, which means that they can give rise to all cell types of the body, but no extraembryonic tissues. During embryo development, embryonic stem cells soon lose their pluripotency as they begin to differentiate into other tissues. Since the 1990s, scientists have been able to extract human embryonic stem cells from the inner cell mass of the blastocyst and grow and study them in the lab.5 This has led to many important discoveries about human embryonic development. Research on human embryos is a matter of constant ethical debate and is even illegal in some countries. In Sweden, many embryonic stem cells used in research come from leftover embryos from in vitro fertilization (IVF) treatments. Researchers are only allowed to use the embryos until they are 14 days old, after which they must be destroyed to stop further development.6
Induced pluripotent stem cells (iPSCs)
It was believed for a very long time that once a cell becomes fully mature, it can never revert back to a stem cell stage. However, in 2006 a group of Japanese scientists discovered that by turning on just four genes, it is possible to create a cell very similar to an embryonic stem cell from a mature cell through a process called reprogramming.7 They named these reprogrammed cells induced pluripotent stem cells, and were awarded the Nobel Prize in 2012 for their ground-breaking research. The ability to create pluripotent stem cells from any kind of mature cell type has led to a lot of new possibilities for researchers to study development without having to use human embryos. Induced pluripotent stem cells can also be used to study disease development and for testing new drugs. In the future, scientists and medical doctors hope to be able to use induced pluripotent stem cells to treat diseases caused by loss of/injury in a particular tissue, such as Parkinson’s disease, multiple sclerosis (MS) and heart failure. However, so far, the use of induced pluripotent stem cells in the clinic is extremely limited and much more research is required before induced pluripotent stem cells can be used to their full potential.
Adult stem cells
These cells reside in different tissues and supply the organism with new cells. They are multipotent, which means they can only differentiate into cells that make up the tissue where they belong. Therefore, they are less potent than embryonic stem cells. An example of adult stem cells are hematopoietic (blood) and neural stem cells.
Read more about hematopoietic stem cells here
Read more about neural stem cells here
Cancer stem cells
Tumor cells that have the ability to self-renew and differentiate are called cancer stem cells. Cancer stem cells were first identified in blood cancer (leukemia) in the late 1990s. The discovery of cancer stem cells has completely changed our understanding of tumor and cancer biology. Because of their ability self-renew and supply the tumor with new cells, cancer stem cells are believed to be one of the main reasons for why cancer often comes back after the patient receives treatment. This means that in order to completely cure a patient from cancer, the treatment must attack the cancer stem cells. Unfortunately, cancer stem cells are not killed by regular cancer treatments such as chemotherapy. Thanks to the effort of many researchers over the past 20 years, several therapies targeting cancer stem cells in different cancers have been developed. These targeted therapies can eliminate the cancer stem cells and typically have fewer side effects compared to chemotherapy, because they are specific to the cancer stem cells and leave other kinds of cells untouched. By continuing the research on cancer stem cells, scientists hope to develop even more specific therapies targeting cancer stem cells that can replace current treatments that are often harmful and dangerous for the patient.8
Future perspectives of stem cell research
Stem cell research is a rather young but constantly growing discipline.9 It has had a large impact on our understanding of biology and medicine. The combination of (stem) cell therapy, gene therapy, and tissue engineering has led to an entirely new field, now known as regenerative medicine.10
However, medical advancements usually follow years of intensive research. Stem cells provide excellent model systems and allow us to study questions such as: How are processes such as homeostasis and differentiation regulated on a cellular level? How are organs built and maintained? How do complex multicellular organisms (including us) develop from a single cell (a fertilized egg cell)? There are many more open questions that are left to be answered by future scientists.
Besides satisfying scientific curiosity, stem cell research holds promising new treatment opportunities for a whole range of diseases, such as cancer, degenerative diseases, or consequences of traumas.11 So far, only a few therapies have made it from the laboratory to the clinics. Some of these approved therapies are: Hematopoietic stem cell transplantation, regeneration therapy of the cornea (the clear outer layer of the eye), and regeneration therapy of the skin following severe burns6. Many more stem cell based therapies are on the way and will be tested in clinical trials in the coming years. The regeneration potential of stem cell based therapies raises the hope to not only treat the symptoms of a disease, but also to restore the affected system entirely. However, it is advisable to be patient. There are many black sheep out there that try to make quick money with premature, unapproved or even harmful “treatments”. Research takes time. After all, it took almost 30 years to translate the above-mentioned therapies from the laboratory to the clinics.10 Therefore, it is recommended to stay suspicious if someone claims to have one miraculous cure for a variety of different diseases. Always keep in mind: If something seems too good to be true, it probably is.